Physical activity in kidney disease: evidence and implementation
Piggin, J. What is physical activity? A holistic definition for teachers, researchers and policy makers. Front. Sports Act. Living 2, 72 (2020).
Google Scholar
Tucker, W. J. et al. Exercise for primary and secondary prevention of cardiovascular disease: JACC focus seminar 1/4. J. Am. Coll. Cardiol. 80, 1091–1106 (2022).
Google Scholar
Caspersen, C. J., Powell, K. E. & Christenson, G. M. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public. Health Rep. 100, 126 (1985).
Google Scholar
Painter, P., Stewart, A. L. & Carey, S. Physical functioning: definitions, measurement, and expectations. Adv. Ren. Replace. Ther. 6, 110–123 (1999).
Google Scholar
Marquez, D. X. et al. A systematic review of physical activity and quality of life and well-being. Transl. Behav. Med. 10, 1098–1109 (2020).
Google Scholar
Strain et al. National, regional, and global trends in insufficient physical activity among adults from 2000 to 2022: a pooled analysis of 507 population-based surveys with 5·7 million participants. Lancet Glob. Health 12, e1232–e1243 (2024).
Google Scholar
Katzmarzyk, P. T., Friedenreich, C., Shiroma, E. J. & Lee, I.-M. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br. J. Sports Med. 56, 101–106 (2022).
Google Scholar
Webster, A. C., Nagler, E. V., Morton, R. L. & Masson, P. Chronic kidney disease. Lancet 389, 1238–1252 (2017).
Google Scholar
Vallianou, N. G., Mitesh, S., Gkogkou, A. & Geladari, E. Chronic kidney disease and cardiovascular disease: is there any relationship? Curr. Cardiol. Rev. 15, 55–63 (2019).
Google Scholar
Wilkinson, T. J. et al. Prevalence and correlates of physical activity across kidney disease stages: an observational multicentre study. Nephrol. Dial. Transplant. 36, 641–649 (2021).
Google Scholar
Kalantar-Zadeh, K., Jafar, T. H., Nitsch, D., Neuen, B. L. & Perkovic, V. Chronic kidney disease. Lancet 398, 786–802 (2021).
Google Scholar
Seidu, S. A. M. et al. Physical activity and risk of chronic kidney disease: systematic review and meta-analysis of 12 cohort studies involving 1,281,727 participants. Eur. J. Epidemiol. 38, 267–280 (2023).
Google Scholar
Castillo-García, A. et al. Physical activity, chronic kidney disease, and cardiovascular risk: a study in half a million adults. Scand. J. Med. Sci. Sports 34, e14557 (2024).
Google Scholar
Zhang, F. et al. Therapeutic effects of exercise interventions for patients with chronic kidney disease: an umbrella review of systematic reviews and meta-analyses. BMJ Open. 12, e054887 (2022).
Google Scholar
Hellberg, M., Höglund, P., Svensson, P. & Clyne, N. Randomized controlled trial of exercise in CKD — the RENEXC study. Kidney Int. Rep. 4, 963–976 (2019).
Google Scholar
Zhou, Y., Hellberg, M., Hellmark, T., Höglund, P. & Clyne, N. Twelve months of exercise training did not halt abdominal aortic calcification in patients with CKD — a sub-study of RENEXC — a randomized controlled trial. BMC Nephrol. 21, 1–10 (2020).
Google Scholar
Weiner, D. E. et al. Effect of long-term exercise training on physical performance and cardiorespiratory function in adults with CKD: a randomized controlled trial. Am. J. Kidney Dis. 81, 59–66 (2023).
Google Scholar
Hayden, C. M., Begue, G., Gamboa, J. L., Baar, K. & Roshanravan, B. Review of exercise interventions to improve clinical outcomes in non-dialysis chronic kidney disease. Kidney Int. Rep. 9, 3097–3115 (2024).
Google Scholar
Graham-Brown, M. P. et al. A randomized controlled trial to investigate the effects of intra-dialytic cycling on left ventricular mass. Kidney Int. 99, 1478–1486 (2021).
Google Scholar
Young, H. M. et al. Exercise for people living with frailty and receiving haemodialysis: a mixed-methods randomised controlled feasibility study. BMJ Open. 10, e041227 (2020).
Google Scholar
March, D. S. et al. A cost-effective analysis of the CYCLE-HD randomized controlled trial. Kidney Int. Rep. 6, 1548–1557 (2021).
Google Scholar
Anding-Rost, K. et al. Exercise during hemodialysis in patients with chronic kidney failure. NEJM Evid. 2, EVIDoa2300057 (2023).
Google Scholar
Tabibi, M. A., Cheema, B., Salimian, N., Corrêa, H. L. & Ahmadi, S. The effect of intradialytic exercise on dialysis patient survival: a randomized controlled trial. BMC Nephrol. 24, 100 (2023).
Google Scholar
Greenwood, S. A. et al. Randomized trial — prescription of intradialytic exercise to improve quality of life in patients receiving hemodialysis. Kidney Int. Rep. 6, 2159–2170 (2021).
Google Scholar
Hu, H., Liu, X., Chau, P. H. & Choi, E. P. H. Effects of intradialytic exercise on health-related quality of life in patients undergoing maintenance haemodialysis: a systematic review and meta-analysis. Qual. Life Res. 31, 1–18 (2022).
Google Scholar
Manfredini, F. et al. Exercise in patients on dialysis: a multicenter, randomized clinical trial. J. Am. Soc. Nephrol. 28, 1259–1268 (2017).
Google Scholar
Mallamaci, F. et al. Long-term effect of physical exercise on the risk for hospitalization and death in dialysis patients: a post-trial long-term observational study. Clin. J. Am. Soc. Nephrol. 17, 1176–1182 (2022).
Google Scholar
Manfredini, F. et al. The legacy effect of a home walking exercise programme in kidney failure patients on dialysis. Nephrol. Dial. Transplant. 37, 1974–1981 (2022).
Google Scholar
Tarca, B. et al. Exercise or physical activity-related adverse events in people receiving peritoneal dialysis: a systematic review. Perit. Dial. Int. 42, 447–459 (2022).
Google Scholar
Thangarasa, T., Imtiaz, R., Hiremath, S. & Zimmerman, D. Physical activity in patients treated with peritoneal dialysis: a systematic review and meta-analysis. Can. J. Kidney Health Dis. 5, 2054358118779821 (2018).
Google Scholar
Bennett, P. N. et al. An exercise program for peritoneal dialysis patients in the United States: a feasibility study. Kidney Med. 2, 267–275 (2020).
Google Scholar
Uchiyama, K. et al. Home-based aerobic exercise and resistance training in peritoneal dialysis patients: a randomized controlled trial. Sci. Rep. 9, 2632 (2019).
Google Scholar
Watanabe, K. et al. Home-based exercise and bone mineral density in peritoneal dialysis patients: a randomized pilot study. BMC Nephrol. 22, 1–9 (2021).
Google Scholar
Luo, Y., Yang, Z., Chen, X. & Huang, Y. Effect of a video-based exercise intervention on depression and sleep conditions of peritoneal dialysis patients. Clin. Nephrol. 99, 58 (2023).
Google Scholar
Bennett, P. N. et al. Physical activity and exercise in peritoneal dialysis: International society for peritoneal dialysis and the global renal exercise network practice recommendations. Perit. Dial. Int. 42, 8–24 (2022).
Google Scholar
Wilkinson, T. J. et al. The effect of exercise training interventions in adult kidney transplant recipients: a systematic review and meta-analysis of randomised control trials. Phys. Ther. Rev. 27, 114–134 (2022).
Google Scholar
Painter, P. L. et al. A randomized trial of exercise training after renal transplantation. Transplantation 74, 42–48 (2002).
Google Scholar
Greenwood, S. A. et al. Aerobic or resistance training and pulse wave velocity in kidney transplant recipients: a 12-week pilot randomized controlled trial (the Exercise in Renal Transplant [ExeRT] Trial). Am. J. Kidney Dis. 66, 689–698 (2015).
Google Scholar
Knobbe, T. J. et al. Effect of an exercise intervention or combined exercise and diet intervention on health-related quality of life – physical functioning after kidney transplantation: the active care after transplantation (ACT) multicentre randomised controlled trial. Lancet Healthy Longev. 5, 100622 (2024).
Google Scholar
McAdams-DeMarco, M., Ying, H. & Van Pilsum Rasmussen, S. Prehabilitation prior to kidney transplantation. Results from a pilot study. Clin. Transplant.33, e13450 (2019).
Google Scholar
Lorenz, E. C. et al. Protocolized exercise improves frailty parameters and lower extremity impairment: a promising prehabilitation strategy for kidney transplant candidates. Clin. Transplant. 34, e14017 (2020).
Google Scholar
Ma, X. et al. Face-to-face mentoring, remotely supervised home exercise prehabilitation to improve physical function in patients awaiting kidney transplantation: a randomized clinical trial. Front. Psychol. 13, 831445 (2022).
Google Scholar
Michou, V. et al. Effects of a combined intradialytic exercise training program on functional capacity and body composition in kidney transplant candidates. J. Funct. Morphol. Kinesiol. 8, 9 (2023).
Google Scholar
Perez-Saez, M. J. et al. The FRAILMar study protocol: frailty in patients with advanced chronic kidney disease awaiting kidney transplantation. A randomized clinical trial of multimodal prehabilitation. Front. Med. 8, 675049 (2021).
Google Scholar
Quint, E. E. et al. Prehabilitation of candidates for renal transplantation (PreCareTx) study: protocol for a hybrid type I, mixed method, randomised controlled trial. BMJ Open. 13, e072805 (2023).
Google Scholar
Greenwood, S. A. et al. Evaluating the effect of a digital health intervention to enhance physical activity in people with chronic kidney disease (Kidney BEAM): a multicentre, randomised controlled trial in the UK. Lancet Digital Health 6, e23–e32 (2024).
Google Scholar
Young, H. M. et al. The development and internal pilot trial of a digital physical activity and emotional well-being intervention (Kidney BEAM) for people with chronic kidney disease. Sci. Rep. 14, 700 (2024).
Google Scholar
Greenwood, S. A. et al. Kidney beam-a cost-effective digital intervention to improve mental health. Kidney Int. Rep. 9, 3204–3217 (2024).
Google Scholar
Lightfoot, C. J. et al. The effects of a digital health intervention on patient activation in chronic kidney disease. NPJ Digit. Med. 7, 318 (2024).
Google Scholar
Stevens, P. E. et al. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 105, S117–S314 (2024).
Google Scholar
National Institute for Health and Care Excellence. Chronic Kidney Disease: Assessment and Management NICE Guideline [NG203]. nice.org (2021).
KD, W. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am. J. Kidney Dis. 45, S1–S153 (2005).
Lambert, K., Lightfoot, C. J., Jegatheesan, D. K., Gabrys, I. & Bennett, P. N. Physical activity and exercise recommendations for people receiving dialysis: a scoping review. PLoS ONE 17, e0267290 (2022).
Google Scholar
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462 (2020).
Google Scholar
Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group KDIGO clinical practice guideline for the care of kidney transplant recipients. Am. J. Transplant. 9, S1–S155 (2009).
Google Scholar
Kasiske, B. L. et al. KDIGO clinical practice guideline for the care of kidney transplant recipients: a summary. Kidney Int. 77, 299–311 (2010).
Google Scholar
Annema, C. et al. European Society of Organ Transplantation (ESOT) consensus statement on prehabilitation for solid organ transplantation candidates. Transpl. Int. 36, 11564 (2023).
Google Scholar
Yamagata, K. et al. Clinical practice guideline for renal rehabilitation: systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Ren. Replace. Ther. 5, 1–19 (2019).
Google Scholar
UK Kidney Association. Clinical Practice Guideline Post-Operative Care in the Kidney Transplant Recipient. ukkidney.org (2017).
Baker, L. A. et al. Clinical practice guideline exercise and lifestyle in chronic kidney disease. BMC Nephrol. 23, 75 (2022).
Google Scholar
Ashby, D. et al. Renal association clinical practice guideline on haemodialysis. BMC Nephrol. 20, 1–36 (2019).
Google Scholar
Kouidi, E. et al. The role of exercise training on cardiovascular risk factors and heart disease in patients with chronic kidney disease G3–G5 and G5D: a clinical consensus statement of the European Association of Preventive Cardiology of the ESC and the European Association of Rehabilitation in Chronic Kidney Disease. Eur. J. Prev. Cardiol. 31, 1493–1515 (2024).
Google Scholar
Tentori, F. et al. Physical exercise among participants in the dialysis outcomes and practice patterns study (DOPPS): correlates and associated outcomes. Nephrol. Dial. Transplant. 25, 3050–3062 (2010).
Google Scholar
Ancliffe, L., Castle, E. M., Wilkinson, T. J. & Young, H. M. A national survey of current rehabilitation service provisions for people living with chronic kidney disease in the UK: implications for policy and practice. BMC Nephrol. 25, 1–13 (2024).
Google Scholar
Bulighin, F. Physical activity and exercise programs for kidney patients: an Italian survey of nephrology centres. J. Nephrol. 37, 695–705 (2024).
Google Scholar
Ma, S., Lui, J., Brooks, D. & Parsons, T. L. The availability of exercise rehabilitation programs in hemodialysis centres in Ontario. CANNT J. 22, 26–32 (2012).
Google Scholar
Barros, F. S. et al. Exercise training during hemodialysis in Brazil: a national survey. Artif. Organs 45, 1368–1376 (2021).
Google Scholar
Villanego, F., Arroyo, D., Martínez-Majolero, V., Hernández-Sánchez, S. & Esteve-Simó, V. Importance of physical exercise prescription in patients with chronic kidney disease: results of the survey of the Grupo Español Multidisciplinar de Ejercicio Físico en el Enfermo Renal [Spanish Multidisciplinary Group of Physical Exercise in Kidney Patients] (GEMEFER). Nefrología 43, 126–132 (2023).
Google Scholar
Molsted, S. et al. Nurses’ and medical doctors’ attitudes towards exercise for people with chronic kidney disease in Denmark. J. Ren. Care 49, 206–216 (2023).
Google Scholar
Taylor, R. S., Dalal, H. M. & McDonagh, S. T. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat. Rev. Cardiol. 19, 180–194 (2022).
Google Scholar
Troosters, T., Janssens, W., Demeyer, H. & Rabinovich, R. A. Pulmonary rehabilitation and physical interventions. Eur. Respir. Rev. 32, 220222 (2023).
Google Scholar
Al Hennawi, H. et al. Impact of exercise training on clinical outcomes and quality of life in chronic congestive heart failure: a systematic review and meta-analysis. Curr. Probl. Cardiol. 49, 102756 (2024).
Google Scholar
Bohm, C. et al. Advancing exercise science for better health outcomes across the spectrum of chronic kidney disease. J. Ren. Nutr. 33, S103–S109 (2023).
Google Scholar
West, R. R., Jones, D. A. & Henderson, A. H. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 98, 637–644 (2012).
Google Scholar
Dibben, G. O. et al. Exercise-based cardiac rehabilitation for coronary heart disease: a meta-analysis. Eur. Heart J. 44, 452–469 (2023).
Google Scholar
Ryrsø, C. K. et al. Lower mortality after early supervised pulmonary rehabilitation following COPD-exacerbations: a systematic review and meta-analysis. BMC Pulm. Med. 18, 1–18 (2018).
Google Scholar
McCarthy, B. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2015, CD003793 (2015).
Google Scholar
Abreu, A. et al. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: the avenue towards EAPC accreditation programme: a position statement of the secondary prevention and rehabilitation section of the European association of preventive cardiology (EAPC). Eur. J. Prev. Cardiol. 28, 496–509 (2021).
Google Scholar
Ambrosetti, M. et al. Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 28, 460–495 (2021).
Google Scholar
Cowie, A. et al. Standards and core components for cardiovascular disease prevention and rehabilitation. Heart 105, 510–515 (2019).
Google Scholar
Coyne, E. et al. Achieving consensus on psychosocial and physical rehabilitation management for people living with kidney disease. Clin. Kidney J. 16, 2185–2193 (2023).
Google Scholar
UK Kidney Association. A Multi-Professional Renal Workforce Plan for Adults and Children with Kidney Disease. ukkidney.org (2020).
Eccles, M. & Mittman, B. Welcome to implementation science. Implement. Sci. 1, 1 (2006).
Google Scholar
Bauer, M. S. & Kirchner, J. Implementation science: what is it and why should I care? Psychiatry Res. 283, 112376 (2020).
Google Scholar
Young, H. M. et al. Patient and staff perceptions of intradialytic exercise before and after implementation: a qualitative study. PLoS ONE 10, e0128995 (2015).
Google Scholar
Young, H. M. et al. Implementing a theory-based intradialytic exercise programme in practice: a quality improvement project. Clin. Kidney J. 11, 832–840 (2018).
Google Scholar
Kilbourne, A. M., Glasgow, R. E. & Chambers, D. A. What can implementation science do for you? Key success stories from the field. J. Gen. Intern. Med. 35, 783–787 (2020).
Google Scholar
Michie, S., Atkins, L. & West, R. The Behaviour Change Wheel: A Guide Designing Interventions (Silverback, 2014).
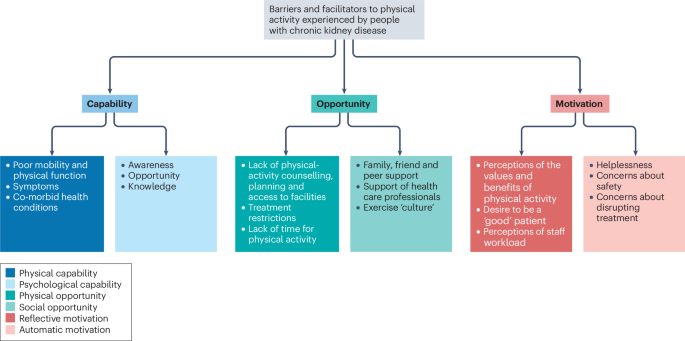
Clarke, A. L., Jhamb, M. & Bennett, P. N. Barriers and facilitators for engagement and implementation of exercise in end-stage kidney disease: future theory-based interventions using the Behavior Change Wheel. Semin. Dial. 32, 308–319 (2019).
Google Scholar
Ross, R. et al. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 45, S57–S102 (2020).
Google Scholar
Davies, M. et al. Hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 45, 2753–2786 (2022).
Google Scholar
Sheshadri, A., Kittiskulnam, P., Lazar, A. A. & Johansen, K. L. A walking intervention to increase weekly steps in dialysis patients: a pilot randomized controlled trial. Am. J. Kidney Dis. 75, 488–496 (2020).
Google Scholar
Lyden, K. et al. Targeting sedentary behavior in CKD: a pilot and feasibility randomized controlled trial. Clin. J. Am. Soc. Nephrol. 16, 717–726 (2021).
Google Scholar
Christensen, J. C. et al. The sit less, interact and move more (SLIMM-2) trial: protocol for a randomized control trial of a sedentary behavior intervention, resistance training and semaglutide on sedentary behavior in persons with chronic kidney disease. Contemp. Clin. Trials 149, 107766 (2025).
Google Scholar
ISRCTN. Tailored 24-Hour Physical Behaviours for People Living with Multiple Cardiorenal Metabolic Conditions and Frailty. isrctn.com (2025).
Dogra, S. et al. Start with reducing sedentary behavior: a stepwise approach to physical activity counseling in clinical practice. Patient Educ. Couns. 105, 1353–1361 (2022).
Google Scholar
Birkeland, S., Bismark, M., Barry, M. J. & Möller, S. Is greater patient involvement associated with higher satisfaction? Experimental evidence from a vignette survey. BMJ Qual. Saf. 31, 86–93 (2022).
Google Scholar
Thompson, S., Tonelli, M., Klarenbach, S. & Molzahn, A. A qualitative study to explore patient and staff perceptions of intradialytic exercise. Clin. J. Am. Soc. Nephrol. 11, 1024–1033 (2016).
Google Scholar
Regolisti, G. et al. Interaction of healthcare staff’s attitude with barriers to physical activity in hemodialysis patients: a quantitative assessment. PLoS ONE 13, e0196313 (2018).
Google Scholar
Martínez-Majolero, V., Urosa, B. & Hernández-Sánchez, S. Physical exercise in people with chronic kidney disease — practices and perception of the knowledge of health professionals and physical activity and sport science professionals about their prescription. Int. J. Environ. Res. Public. Health 19, 656 (2022).
Google Scholar
Bulley, C. et al. Feasibility of randomized controlled trials and long-term implementation of interventions: insights from a qualitative process evaluation of the PEDAL trial. Front. Rehabil. Sci. 4, 1100084 (2023).
Google Scholar
Painter, P., Clark, L. & Olausson, J. Physical function and physical activity assessment and promotion in the hemodialysis clinic: a qualitative study. Am. J. Kidney Dis. 64, 425–433 (2014).
Google Scholar
Taryana, A. A. et al. Physical activity for people with chronic kidney disease: an international survey of nephrologist practice patterns and research priorities. BMJ Open. 9, e032322 (2019).
Google Scholar
Anding, K. et al. A structured exercise programme during haemodialysis for patients with chronic kidney disease: clinical benefit and long-term adherence. BMJ Open. 5, e008709 (2015).
Google Scholar
Jhamb, M. et al. Knowledge, barriers and facilitators of exercise in dialysis patients: a qualitative study of patients, staff and nephrologists. BMC Nephrol. 17, 1–14 (2016).
Google Scholar
Castillo, G. et al. Addressing feasibility challenges to delivering intradialytic exercise interventions: a theory-informed qualitative study. Nephrol. Dial. Transplant. 37, 558–574 (2022).
Google Scholar
Fiaccadori, E. et al. Barriers to physical activity in chronic hemodialysis patients: a single-center pilot study in an Italian dialysis facility. Kidney Blood Press. Res. 39, 169–175 (2014).
Google Scholar
Michou, V., Kouidi, E., Liakopoulos, V., Dounousi, E. & Deligiannis, A. Attitudes of hemodialysis patients, medical and nursing staff towards patients’ physical activity. Int. Urol. Nephrol. 51, 1249–1260 (2019).
Google Scholar
Li, T. et al. Barriers and facilitators to exercise in haemodialysis patients: a systematic review of qualitative studies. J. Adv. Nurs. 77, 4679–4692 (2021).
Google Scholar
Williams, A. D., Fassett, R. G. & Coombes, J. S. Exercise in CKD: why is it important and how should it be delivered? Am. J. Kidney Dis. 64, 329–331 (2014).
Google Scholar
Teo, R. Z. C., Kaur, D., Ong, D., Singh, T. & Khan, B. A. Implementation of exercise therapy in kidney failure. Ren. Soc. Australas. J. 18, 9–14 (2022).
Delgado, C. & Johansen, K. L. Deficient counseling on physical activity among nephrologists. Nephron Clin. Pract. 116, c330–c336 (2010).
Google Scholar
Bennett, P. N. et al. Sustaining a hemodialysis exercise program: a review. Semin. Dial. 23, 62–73 (2010).
Google Scholar
Miller W. & Rollnick S. Motivational Interviewing: Facilitating Change, 3rd edn (Guilford Press, 2012).
van Vilsteren, M. C., de Greef, M. H. & Huisman, R. M. The effects of a low-to-moderate intensity pre-conditioning exercise programme linked with exercise counselling for sedentary haemodialysis patients in The Netherlands: results of a randomized clinical trial. Nephrol. Dial. Transplant. 20, 141–146 (2005).
Google Scholar
Wodskou, P. M., Reinhardt, S. M., Andersen, M. B., Molsted, S. & Schou, L. H. Motivation, barriers, and suggestions for intradialytic exercise — a qualitative study among patients and nurses. Int. J. Environ. Res. Public. Health 18, 10494 (2021).
Google Scholar
Bennett, P. N. et al. An international survey of peritoneal dialysis exercise practices and perceptions. Kidney Int. Rep. 8, 1389–1398 (2023).
Google Scholar
Capitanini, A. et al. Dialysis exercise team: the way to sustain exercise programs in hemodialysis patients. Kidney Blood Press. Res. 39, 129–133 (2014).
Google Scholar
Müller-Ortiz, H. et al. Recommendations for implementation of physical training guidelines for patients undergoing chronic hemodialysis. J. Hum. Sport Exercise (2021).
Viana, J. L. et al. Sustained exercise programs for hemodialysis patients: the characteristics of successful approaches in Portugal, Canada, Mexico, and Germany. Semin. Dial. 32, 320–330 (2019).
Google Scholar
Wang, Y. et al. A scoping review of implementation science theories, models, and frameworks — an appraisal of purpose, characteristics, usability, applicability, and testability. Implement. Sci. 18, 43 (2023).
Google Scholar
Meza, R. D. et al. Theorizing is for everybody: advancing the process of theorizing in implementation science. Front. Health Serv. 3, 1134931 (2023).
Google Scholar
Kislov, R., Pope, C., Martin, G. P. & Wilson, P. M. Harnessing the power of theorising in implementation science. Implement. Sci. 14, 1–8 (2019).
Google Scholar
Nilsen, P. Making sense of implementation theories, model, and frameworks. Implement. Sci. 10, 53–79 (2020).
Google Scholar
May, C. R. et al. Development of a theory of implementation and integration: normalization process theory. Implement. Sci. 4, 1–9 (2009).
Google Scholar
May, C. R. et al. Using normalization process theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement. Sci. 13, 1–27 (2018).
Google Scholar
Glasgow, R. E., Vogt, T. M. & Boles, S. M. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am. J. Public. Health 89, 1322–1327 (1999).
Google Scholar
Birken, S. A. et al. Criteria for selecting implementation science theories and frameworks: results from an international survey. Implement. Sci. 12, 1–9 (2017).
Google Scholar
Proctor, E. K., Powell, B. J., Baumann, A. A., Hamilton, A. M. & Santens, R. L. Writing implementation research grant proposals: ten key ingredients. Implement. Sci. 7, 1–13 (2012).
Google Scholar
Moullin, J. C. et al. Ten recommendations for using implementation frameworks in research and practice. Implement. Sci. Commun. 1, 1–12 (2020).
Google Scholar
Stover, A. M. et al. Using an implementation science approach to implement and evaluate patient-reported outcome measures (PROM) initiatives in routine care settings. Qual. Life Res. 30, 3015–3033 (2021).
Google Scholar
Strifler, L., Barnsley, J. M., Hillmer, M. & Straus, S. E. Identifying and selecting implementation theories, models and frameworks: a qualitative study to inform the development of a decision support tool. BMC Med. Inform. Decis. Mak. 20, 1–12 (2020).
Google Scholar
Kuek, A. & Hakkennes, S. Healthcare staff digital literacy levels and their attitudes towards information systems. Health Inform. J. 26, 592–612 (2020).
Google Scholar
Arias López, M. D. P. et al. Digital literacy as a new determinant of health: a scoping review. PLoS Digital Health 2, e0000279 (2023).
Google Scholar
Murray, E. et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med. 8, 1–11 (2010).
Google Scholar
de Souto Barreto, P., Ferrandez, A.-M. & Saliba-Serre, B. Are older adults who volunteer to participate in an exercise study fitter and healthier than nonvolunteers? The participation bias of the study population. J. Phys. Act. Health 10, 359–367 (2013).
Google Scholar
Skivington, K., Matthews, L., Craig, P., Simpson, S. & Moore, L. Developing and evaluating complex interventions: updating medical research council guidance to take account of new methodological and theoretical approaches. Lancet 392, S2 (2018).
Google Scholar
May, C. et al. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Serv. Res. 7, 1–7 (2007).
Google Scholar
Greenwood, S. A. et al. Evaluation of a pragmatic exercise rehabilitation programme in chronic kidney disease. Nephrol. Dial. Transplant. 27, iii126–iii134 (2012).
Google Scholar
Martins, P. et al. MO607: intradialytic exercise: a large-scale nationwide implementation study. Nephrol. Dial. Transplant. 37, gfac075 (2022).
Google Scholar
March, D. S. et al. The effect of non-pharmacological and pharmacological interventions on measures associated with sarcopenia in end-stage kidney disease: a systematic review and meta-analysis. Nutrients 14, 1817 (2022).
Google Scholar
Mendoza-Vasconez, A. S. et al. Promoting physical activity among underserved populations. Transl. J. Am. Coll. Sports Med. 1, 125–132 (2016).
Mayes, J. et al. Cultural influences on physical activity and exercise beliefs in patients with chronic kidney disease: ‘The Culture-CKD Study’ — a qualitative study. BMJ Open. 12, e046950 (2022).
Google Scholar
Crocker, J. C. et al. Impact of patient and public involvement on enrolment and retention in clinical trials: systematic review and meta-analysis. BMJ 363, k4738 (2018).
Google Scholar
Patient-Focused Medicine. Making Systematic Patient Engagement a Reality. patientfocusedmedicine.org (2024).
Mullins, C. D., Abdulhalim, A. M. & Lavallee, D. C. Continuous patient engagement in comparative effectiveness research. JAMA 307, 1587–1588 (2012).
Google Scholar
NIH Pragmatic Trials Collaboratory. Patient Engagement Throughout a PCT. rethinkingclinicaltrials.org (2024).
Curran, G. M., Bauer, M., Mittman, B., Pyne, J. M. & Stetler, C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med. Care 50, 217–226 (2012).
Google Scholar
Roundtable on Translating Genomic-Based Research for Health; Board on Health Sciences Policy; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine Applying an Implementation Science Approach to Genomic Medicine: Workshop Summary (National Academies Press, 2016).
Iyasere, O., Young, H. M. & Burton, J. O. Peritoneal dialysis and the role of exercise training interventions. Kidney Dial. 2, 57–67 (2022).
Google Scholar
Beetham, K. S. et al. Effect of a 3-year lifestyle intervention in patients with chronic kidney disease: a randomized clinical trial. J. Am. Soc. Nephrol. 33, 431–441 (2022).
Google Scholar
National Institute for Health and Care Excellence Research. NICE Health Technology Evaluation: The Manual. nice.org (2022).
Damschroder, L. J. et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement. Sci. 4, 1–15 (2009).
Google Scholar
Damschroder, L. J., Reardon, C. M., Widerquist, M. A. O. & Lowery, J. The updated consolidated framework for implementation research based on user feedback. Implement. Sci. 17, 75 (2022).
Google Scholar
Waltz, T. J., Powell, B. J., Fernández, M. E., Abadie, B. & Damschroder, L. J. Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implement. Sci. 14, 1–15 (2019).
Google Scholar
Savaya, R. & Waysman, M. The logic model: a tool for incorporating theory in development and evaluation of programs. Adm. Soc. Work. 29, 85–103 (2005).
Google Scholar
Smith, J. D., Li, D. H. & Rafferty, M. R. The implementation research logic model: a method for planning, executing, reporting, and synthesizing implementation projects. Implement. Sci. 15, 1–12 (2020).
Google Scholar
Glasgow, R. E. et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front. Public. Health 7, 64 (2019).
Google Scholar
Feldstein, A. C. & Glasgow, R. E. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt. Comm. J. Qual. Patient Saf. 34, 228–243 (2008).
Google Scholar
Rabin, B. A. et al. A citation analysis and scoping systematic review of the operationalization of the practical, robust implementation and sustainability model (PRISM). Implement. Sci. 17, 62 (2022).
Google Scholar
link







